Surgery
Click here for Minimally Invasive Surgery
If nonsurgical treatment options have failed, or if there are emergency symptoms, spine surgery may be necessary.The spine surgeons at Quincy Spine Center each perform a high volume of spine surgery each year—typically well over 200 cases annually. They are also fellowship-trained (the highest level of training possible) and board-certified. They concentrate their practice exclusively on spine surgery. Their expertise includes minimally invasive spine surgery, all common surgical problems in the neck and low back, scoliosis surgery, as well as new innovations including total disc replacement. In addition, the surgeons at Quincy Spine Center are already referred some of the most complex spine cases across the region and have extensive experience with cervical myelopathy, scoliosis and deformity surgery as well as revision surgery. This experience translates into improved patient care of all spinal problems.
The following is a list of common surgical problems and issues.
Common spine issues
Cervical Spine (Neck) | Lumbar Spine (Low Back) | Scoliosis | Spinal Fusion | Artificial disc
Cervical Spine / Neck
Discectomy is the removal of the herniated portion of a disc to relieve the pressure on nearby nerves as they exit the spinal canal. Contrary to myths, the disc does not slip out of position like a watermelon seed. Instead, the disc is like a jelly donut, acting as the functional shock absorber between two bony vertebrae. An injury, damage from a lifting incident or a twist may cause the jelly center to break through the wall of the disc. When a disc herniates, the jelly center can press on nearby nerves. In the neck, this causes arm, shoulder, scapula and, in extreme cases, spinal cord compression.

Posterior Cervical Foraminotomy / Discectomy
For some herniated discs or bone spurs in the neck affecting only the nerve roots, a posterior discectomy and foraminotomy can be performed. This avoids spinal fusion, and with a microscope or a minimally invasive technique, can minimize recovery time and speed a patient back to work or activities.
Anterior Cervical Discectomy
Cervical is the medical term for "neck." Just as in a lumbar discectomy, the surgeon will remove a piece of damaged disc tissue in the neck area to relieve pressure on the spinal cord or nerve roots. In some cases, by removing a piece of the shock-absorbing disc that separates the two vertebrae, the structures may become less stable. Consequently, when the disc is removed, a surgeon may recommend "fusing" the vertebrae to prevent instability. A cervical discectomy is best left to surgeons who specialize in spine.
Corpectomy
A corpectomy is often performed for patients suffering from multiple levels of cervical stenosis with cord compression. The goal of a corpectomy is complete decompression of the spinal canal when stenosis encompasses more than just disc space and has moved into vertebral bodies.
Bone spurs forming toward the back of a vertebral body or the ligament behind vertebral bodies can cause the cervical spinal canal to narrow. Therefore, it may be necessary to remove one or more degenerating vertebrae and the discs above and below in order to decompress the spinal cord and nerve roots.
A corpectomy involves a vertical incision in the neck. The middle portion of the vertebra and its adjacent discs are removed to achieve decompression of the cervical spinal cord and nerve roots. A fusion accompanies a corpectomy surgery, using bone harvested from the patient's hip or from a bone bank. This bone graft is used to reconstruct the spine and provide stability.
Anterior Cervical Fusion
A fusion accompanies a anterior cervical discectomy or corpectomy. During fusion surgery, a disc Is removed, and the surgeon inserts a small wedge of bone between two vertebrae to restore disc space. Over time, the two vertebrae "fuse" together into a single solid structure. While this procedure limits movement and flexibility, it also helps relieve neck pain.
Bone graft for the purpose of spinal fusion may be harvested from the patient's hip (autograft bone), from a cadaver bone (allograft bone), or from synthetic bone graft substitutes, which are currently being developed more extensively. Your surgeon will help you decide what is best for you.
Laminoplasty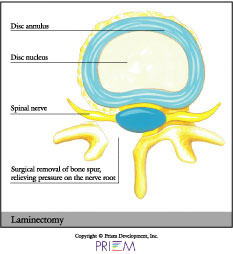
A laminoplasty, similar to a laminectomy, is often performed on patients
suffering from spinal stenosis in the neck (narrowing of the cervical
spinal canal). It is also referred to as an "open-door laminoplasty." A
laminoplasty creates more space for the spinal cord and roots. The
actual procedure involves cutting a “hinge” into one
side of the lamina and swinging it open like a door. It relieves
pressure on the spinal cord by increasing the diameter of the spinal
canal and room for the spinal cord. The surgery approach is through
the back of the neck. This procedure creates excellent spinal canal
decompression without the instability that may be created by multiple
level cervical laminectomies.
[top]
Lumbar surgery/low back
Microdiscectomy / Minimally invasive discectomy
Discectomy is the removal of the herniated portion of a disc to relieve the pressure on nearby nerves as they exit the spinal canal. Contrary to myths, the disc does not slip out of position like a watermelon seed. Instead, the disc is like a jelly donut, acting as the functional shock absorber between two bony vertebrae. An injury, damage from a lifting incident, or a twist may cause the jelly center to break through the wall of the disc. When a disc herniates, the jelly center can press on nearby nerves. This causes back or leg pain when the hernation is in the low back, and arm pain if the disc is in the neck area (see "cervical spine/neck").
 In a lumbar discectomy, the surgeon typically only removes
the portion of the disc that is causing a problem, not the entire disc.
If you have a herniated disc, keep in mind that a disc has a purpose.
When you remove a disc, it may cause instability in the joint, and
a surgeon may recommend a fusion to re-stabilize the area.
In a lumbar discectomy, the surgeon typically only removes
the portion of the disc that is causing a problem, not the entire disc.
If you have a herniated disc, keep in mind that a disc has a purpose.
When you remove a disc, it may cause instability in the joint, and
a surgeon may recommend a fusion to re-stabilize the area.
The surgeon can remove the damaged piece of disc through a traditional incision in the back. However, at Quincy Spine Center, the surgeons typically use a microscope to minimize incision size, tissue trauma and recovery time. In addition, in some cases, minimally invasive discectomy can provide an even less invasive approach.
Depending on the nature of your disc problem, your surgeon will recommend the most appropriate type of surgery for you.
Anterior lumbar interbody fusion (ALIF)
In this type of spinal fusion surgery, back muscles and nerves remain undisturbed. The space between discs is fused by approaching the spine through the abdomen. This procedure is used when the spine is relatively stable, when there's a significant amount of disc space collapse, and in cases of one or two level degenerative disc disease. The surgeon will approach the abdomen through an incision (minilaparotomy) or by using an endoscope.
Posterior lumbar interbody fusion (PLIF)
 This spinal fusion surgery is very similar to the anterior lumbar interbody
fusion, except that the surgeon approaches the spine through the low
back. This method is used when there is a greater amount of instability
in the patient's spine. An advantage to this surgery is that it can
also provide anterior fusion of the disc space without having a second
incision.
This spinal fusion surgery is very similar to the anterior lumbar interbody
fusion, except that the surgeon approaches the spine through the low
back. This method is used when there is a greater amount of instability
in the patient's spine. An advantage to this surgery is that it can
also provide anterior fusion of the disc space without having a second
incision.
Lumbar laminectomy
A laminectomy involves the removal of part or all of the bone covering the spinal canal. The purpose of this procedure can be to free nerve roots, remove a tumor, bone spur or to perform certain types of fusion procedures. Removing the lamina (laminectomy) is much like removing the cover on a fuse box to access the wiring. By removing the lamina, the surgeon gains access to the disc area and frees more space for the nerves inside.
A laminectomy in the lumbar spine is often used to treat
recurrent disc herniations or where scar tissue is involved. Laminectomy
may also be used in cases of spinal stenosis in which the entire canal
is narrowed like a ring on a swollen finger, squeezing all of the nerve
roots at that level of the spinal canal.
[top]
Scoliosis & spinal deformity surgery
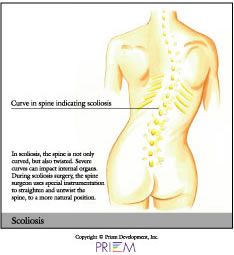 Through the placement of hooks, rods and screws, a spinal curve can
be corrected and stabilized. A fusion often follows scoliosis surgery,
in order to maintain the correction permanently.
Through the placement of hooks, rods and screws, a spinal curve can
be corrected and stabilized. A fusion often follows scoliosis surgery,
in order to maintain the correction permanently.
Scoliosis is not the result of an injury and usually appears without cause. It can be inherited, and it usually affects more women than men. In the case of most spinal curves, the spine is not only bent but also twisted like a bent corkscrew. Some cases of scoliosis are not serious. Over time, if a curve worsens, surgery may be required to correct the curve and prevent pain and worsening deformity. In extreme cases, if the curve is not corrected, the spinal deformity can place pressure on internal organs, which can shorten a person's life expectancy.
During scoliosis surgery, the surgeon may use special
instruments that attach onto various vertebra segments. These surgical
rods are the adjusted to "de-rotate" the twisted and bent
corkscrew spine. Decades ago, Harrington Rods (the “first-generation” of
instrumentation) were used to surgically straighten the spine. However,
this technique did not untwist or correct the spine. Today, there are “fourth-generation” techniques
to improve corrections, minimize levels fused and minimize the need
for post-operative bracing.
[top]
Spinal fusion
Unusual movement at a vertebral segment will probably result in pain, especially if the person already has or displays symptoms of degenerative disc disease, fractures, scoliosis or a weak spine. This movement may require a discectomy, and subsequently, a lumbar interbody fusion. Anterior and posterior fusion techniques can be performed in the neck and the low back.
Not all patients who have spinal problems need spine surgery. They can be managed with microscopic decompression or minimally invasive techniques. Spinal fusion is reserved for patients who have spinal instability, spinal deformity or painful degenerative pain. Obviously, this is only after a patient has failed all conservative measures.
In fusion surgery, the goal is to cause bone graft to
grow between two vertebrae and stop the motion at a particular segment
by adding bone graft to it. This results in one long bone rather than
two separate vertebrae. Anterior and posterior lumbar fusions may be
done separately or can be used together for the most severe problems
of the cervical (neck), thoracic (chest level) and lumbar spine (low
back). Your spinal surgeon will help you decide which technique is
right for you.
[top]
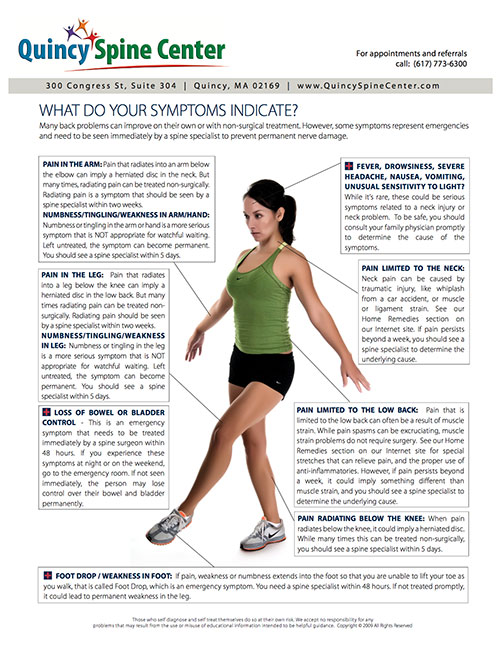
Understanding Symptoms
Pain is not a good indicator of when to see a doctor for a spine problem. While a back spasm can be excruciating, the good news is that ligament strain doesn’t require surgery.
Quincy Bundled Rate
Find out more about a simple 20 minute office procedure — at a $700 bundled rate — that can eliminate the need for spine surgery.

Jeffrey Jackel, MD
Board-certified Anesthesiologist
Board-certified in Pain Medicine (exp)


